It’s well known that hearing damage may be caused by exposure to loud noise, and that the degree of damage is more severe the longer the period of exposure is to noise. What may not be common knowledge is that there is strong evidence that some chemicals (known as ototoxicants) including medicinal drugs could cause hearing loss or imbalance when exposed to them. These effects are independent of noise and may be either temporary or permanent.
It therefore follows that exposure to both noise and ototoxic substances elevate the risk of hearing loss, and this needs to be recognised when carrying out a noise risk assessment.
How is the hearing mechanism affected by ototoxic substances?
Ototoxicants may enter the body by inhalation, ingress through the skin, or ingestion, and eventually find its way into the bloodstream. It may then damage the inner ear by either affecting the structures in the ear itself, or by affecting the nervous system. Some of these ototoxicants may damage the hair cells in the cochlea (i.e. the auditory receptor located in the inner ear) where the hair cells are responsible for transmitting signals to the brain along the auditory nerve. These type of ototoxicants may be classified as cochleotoxicants. There are 2 further types of ototoxicants, viz: neurotoxicants which can inflict auditory damage via the central and peripheral nervous system, and vestibulotoxicants which affect the balance sensors in the ear and result in imbalance. This may be accompanied by dizziness and vertigo.
The detrimental effect of some ototoxic substances upon hearing is that in addition to sounds needing to be louder for detection, it creates both the inability to localise auditory signals and poor frequency resolution which contribute to further hearing impairment. Consequently, in noisy environments, the chances of accidents are heightened for those affected.
Which substances are ototoxic?

Current investigative work into the interaction of ototoxic chemicals with noise is limited and is based on epidemiological studies from humans and also animal research. Where data has been taken from animals exclusively and research bodies have considered the test methods to be robust and reliable, there is a high degree of confidence that the tested substances may be regarded as ototoxic.
Ototoxicity may be present in the following groups of substances. Some of these substances may not be out of place in industrial type environments. The lists are by no means exhaustive:
Solvents
- Styrene and methylstyrene
- Trichloroethylene
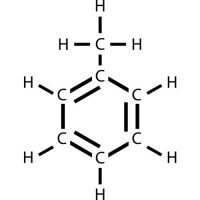
- n-propylbenzene
- Toluene
- Xylene and p-Xylene
- Ethylbenzene
- Carbon disulphide
Asphyxiants
- Hydrogen Cyanide
- Carbon monoxide
Nitriles
- 3 Butenenitrile
- cis-2-pentenenitrile
- acrylonitrile
- cis-crotononitrile
- 3,3 iminodipropionitrile
Metals and compounds
- Lead
- Germanium Dioxide
- Mercury
Medication
- Aminoglysocidic antibiotics (e.g. streptomycin, gentamycin, amikacin)
- Analgesics and antipyretics (e.g. chloroquinine, quinine and salicylates)
- Loop diuretics (e.g. furosemide)
- Chemotherapy agents (e.g. cisplatin, bleomycin, and carboplatin)
Of the medication, ototoxicity may be temporary and mild in small doses but the effect may be more pronounced with consumption of some of the chemotherapy agents used in managing cancer. With an ageing working population, employees could be under such medication regimes.
Which are the high-risk industries?
These are some examples of industries where ototoxic substances are used, and where noise levels can be high, therefore increasing hearing loss risks.
- Fabricated metal manufacture
- Aircraft refuelling
- Textile manufacture
- Furniture building
- Printing
- Paint manufacture
- Construction
- Boat/Ship building
- Chemical production
- Firefighting
- Paint production
- Defence (weapon discharge)
- Leather production
- Solar cell manufacture
- Mining
How can ototoxicants be identified in the workplace?

Research bodies have concluded that current studies do not provide enough robust evidence to be able to publish a dose-effect combined relationship of noise with ototoxicants. Neither The Control of Substances Hazardous to Health Regulations (CoSHH) 2002 nor the Workplace Exposure Limits (EH40/2005) refer to ototoxicity. It’s therefore highly unlikely, for commercial reasons, that manufacturers will warn of ototoxicity on their products. This makes ototoxicants difficult to identify and therefore to apply methods of risk control. The best clue for ototoxicity would be to look out for the word neurotoxic on the product labelling or the safety data sheets.
How do you reduce the aggravation of hearing loss with ototoxicants present?
Some suggested risk mitigative actions employers should consider carrying out in a noisy workplace where staff are in contact with ototoxic substances are listed below.
- Replacing ototoxic chemicals by less ototoxic ones or ones that are not ototoxic.
- Isolating the process from the noisy environment if use of the ototoxicant cannot be avoided.
- Providing information in the risks, hazards, and effects of ototoxic chemicals with noise to employees.
- Increasing the frequency of health surveillance for staff exposed to noise and ototoxicants.
- Providing adequate ventilation and effective PPE in areas where ototoxicants are used.
- Raising staff awareness in the effect of ototoxicant medication upon hearing, and for them to inform their doctors/pharmacist of any concerns.
- Introducing any noise control measures against slightly reduced regulatory exposure limits.
Satish Lakhiani
See www.esselacoustics.com Email: satish@esselacoustics.com